2023-08-24
Abstract
The clinical characteristics of respiratory infectious diseases are mostly fever and (or) respiratory symptoms, the etiological composition is complex, and the selection of specimen types is diverse. How to early and correctly identify patients with potential respiratory infectious diseases from patients with fever and respiratory syndrome is a key link in prevention and control. For patients with lower respiratory tract infection, the types of samples commonly used for pathogenic detection are mainly sputum and alveolar lavage fluid. During the novel coronavirus epidemic, collecting nasopharyngeal swab samples for pathogenic detection of patients with new coronary pneumonia has been proven to have a high diagnostic accuracy, but whether this method is suitable for diagnosing pneumonia caused by other viral infections is still inconclusive.
Recently, an article titled "Agreement of respiratory viruses' detection between nasopharyngeal swab and bronchoalveolar lavage in adults admitted for pneumonia: a retrospective study" was published in the journal Clinical Microbiology and Infection (impact factor 14.2). The consistency of detection of non-new coronaviruses in nasopharyngeal swabs and alveolar lavage fluid of patients with pneumonia was compared and analyzed.

Methods
A retrospective analysis was performed in one French academic hospital on consecutive adults from 2012 to 2018 and tested nasopharyngeal swab and BAL within 24 hours by using multiplex PCR. The agreement in pathogen detection between nasopharyngeal swab and BAL was evaluated.
Results
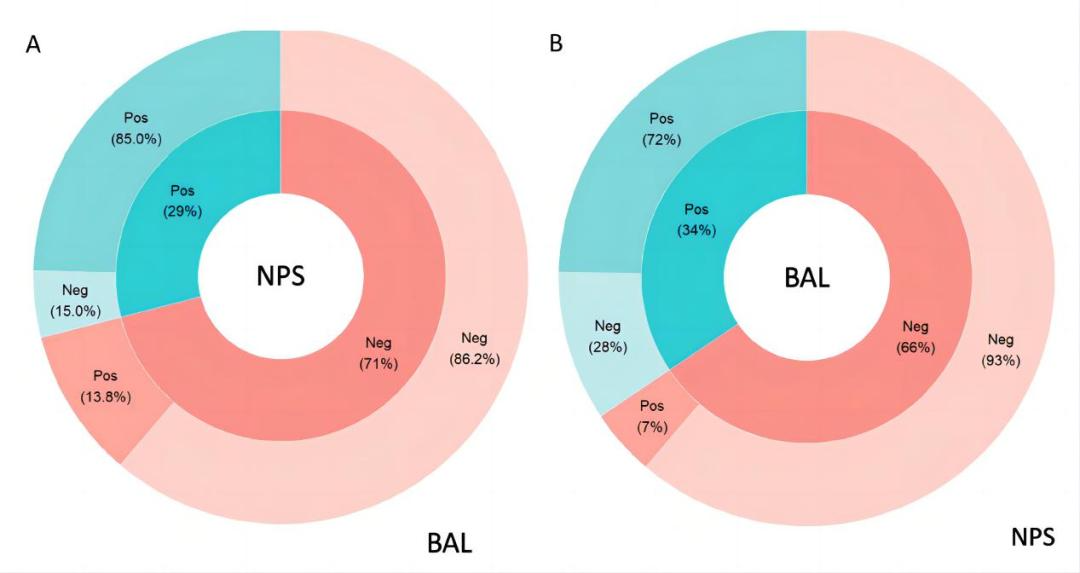
Comparison of overall pathogens detection: Among 276 patients, respiratory viruses were detected in nasopharyngeal swabs and/or alveolar lavage fluid in 107 cases. The virus detection of nasopharyngeal swab samples of 80 patients was positive (29%), and the corresponding positive cases of alveolar lavage fluid samples were 68 (85%); the virus detection of nasopharyngeal swab samples of 196 patients was negative ( 71%), corresponding to 27 positive cases (13.8%) in BALF samples. BALF samples from 95 patients tested positive for virus (34%), and the corresponding number of positive cases in nasopharyngeal swab samples was 68 (72%); BAL fluid samples from 181 patients tested negative for virus ( 66%), and the corresponding number of positive cases in nasopharyngeal swab samples was 12 (7%).
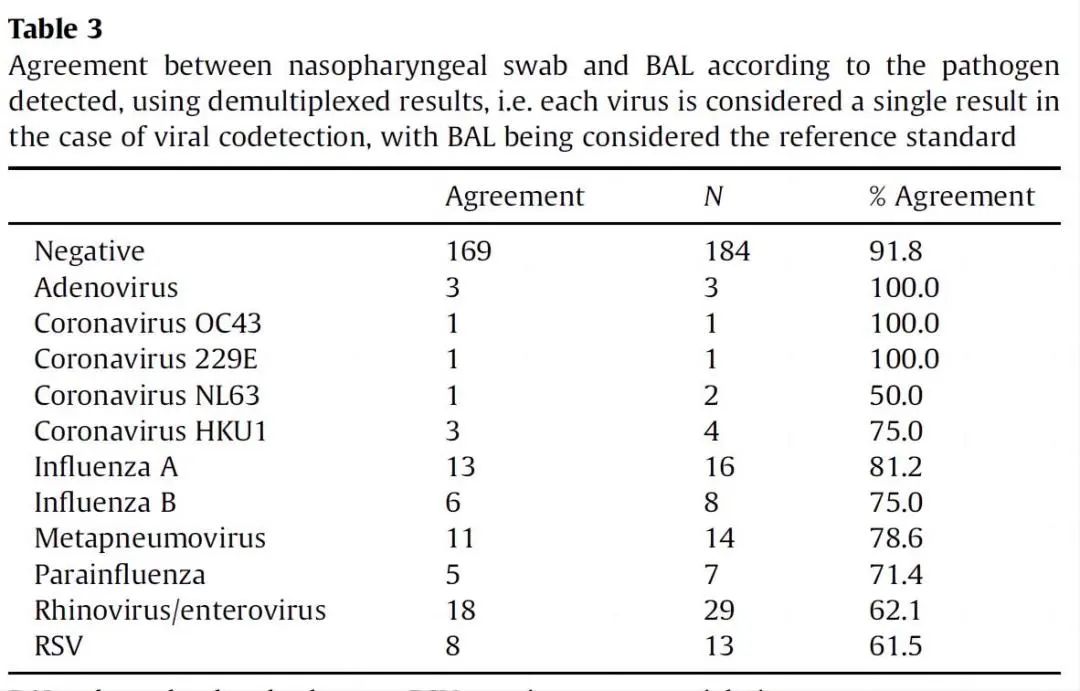
Comparison of detection consistency of different viruses: Taking the test results of bronchoalveolar lavage fluid samples as a reference, the detection consistency of different viruses in nasopharyngeal swabs is shown in the table below. Three cases of adenovirus (Adenovirus), one case of human coronavirus OC43 (Coronavirus OC43) and one case of human coronavirus 229E (Coronavirus 229E) were detected simultaneously in nasopharyngeal swabs, that is, the detection consistency was 100%. The detection consistency of Influenza A virus was 81.2%, while the human coronavirus HKU1 (Coronavirus HKU1), influenza B virus (Influenza B), human metapneumovirus (Metapneumovirus), human parainfluenza virus (Parainfluenza) Consistency is between 70-80%. The identity of rhinovirus (Rhinovirus) and human respiratory syncytial virus (RSV) is about 62%, and the identity of human coronavirus NL63 (Coronavirus NL63) is only 50%.
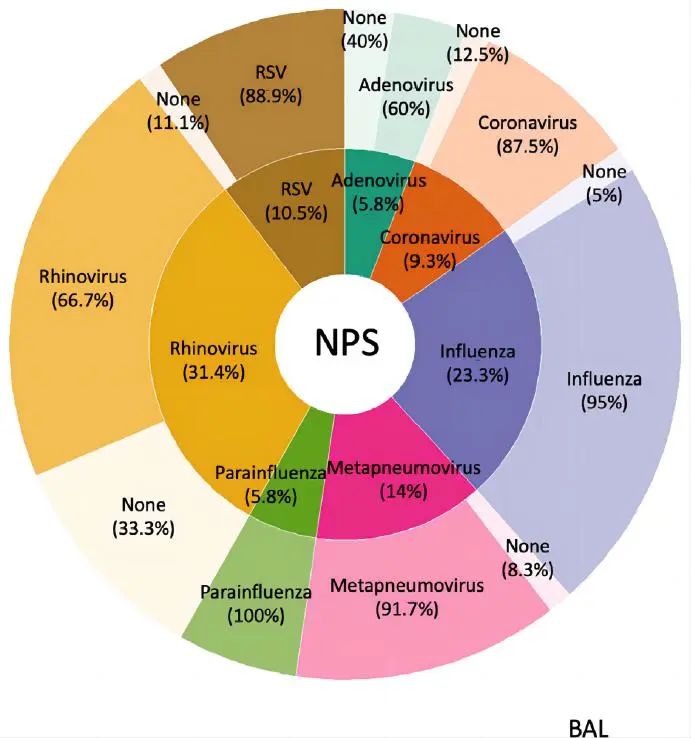
If the test results of nasopharyngeal swab samples are used as a reference, the consistency of detection of different viruses in alveolar lavage fluid is shown in the figure below. The identity of human parainfluenza virus, influenza A/B virus and human metapneumovirus is more than 90%, the identity of respiratory syncytial virus and human coronavirus is about 88%, and the identity of rhinovirus is 66.7%. The virus is only 60%.
Conclusions
There was a good agreement between nasopharyngeal swabs and BAL in detecting respiratory viruses among adult patients with suspected pneumonia. However, these data still encourage BAL in the case of a negative nasopharyngeal swab.
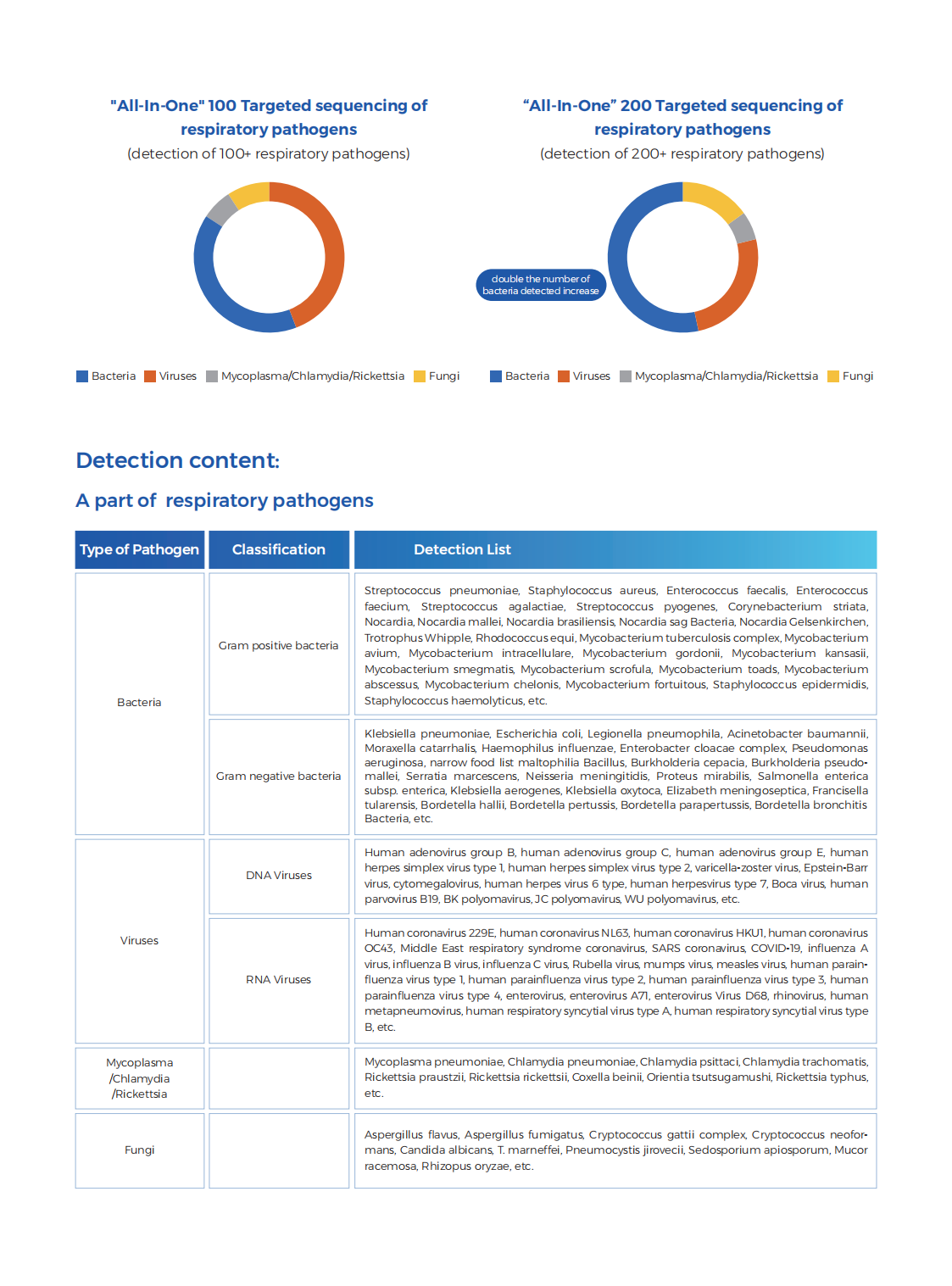
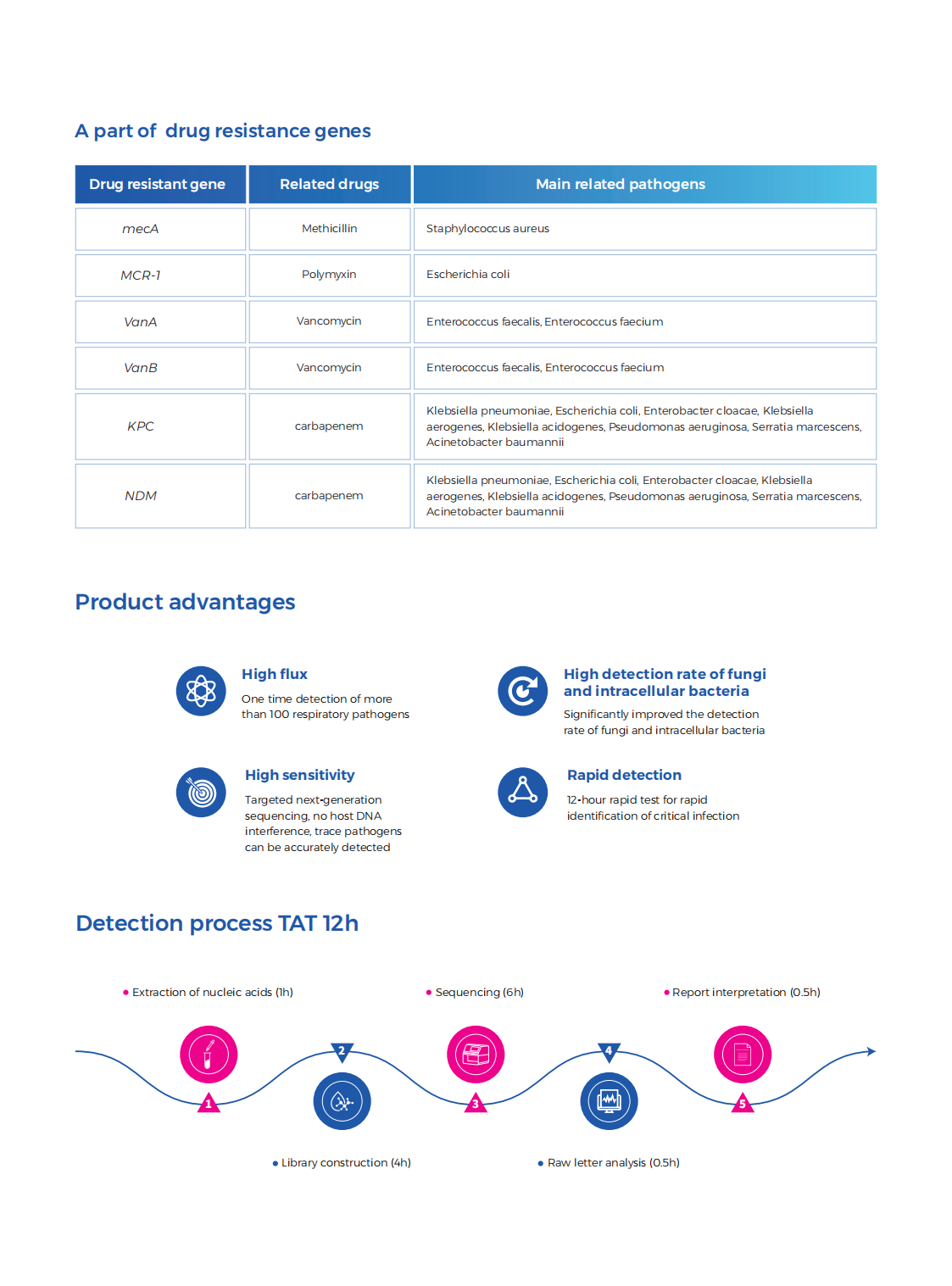
Related Products